Adenomyosis: Why It Causes Painful & Heavy Periods — A Common Problem During Menstruation
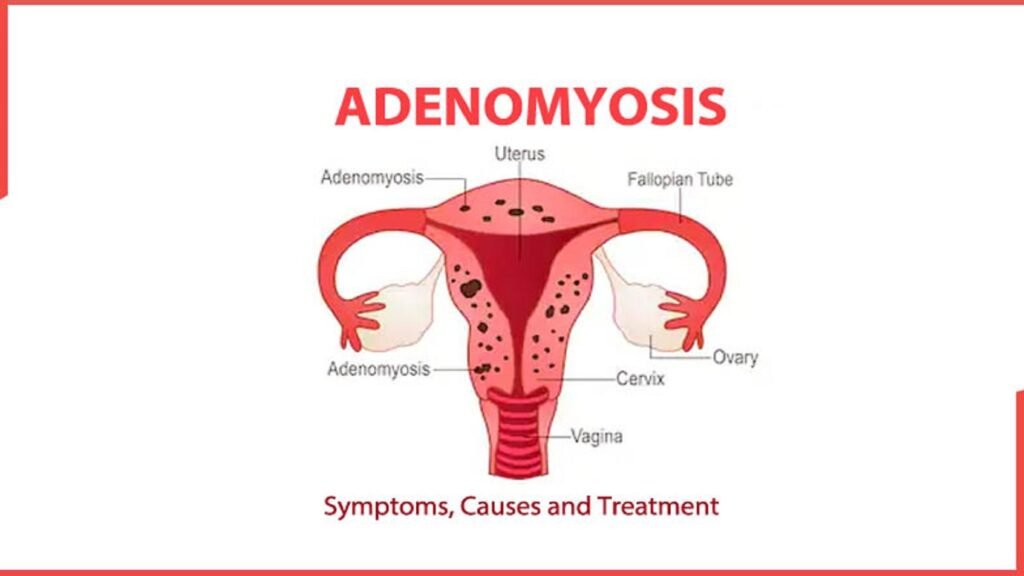
Adenomyosis happens when tissue similar to the uterine lining (endometrium) grows into the muscular wall of the uterus (myometrium). That displaced tissue still responds to menstrual hormones — it thickens, breaks down and bleeds with each cycle — but because it’s trapped inside muscle, it causes swelling, cramping, heavier bleeding and chronic ache for many women.
2. Who gets it and why it matters
Adenomyosis most often appears in women in their 30s and 40s, though it can occur earlier or later. People who’ve had pregnancies may be at higher risk, but it’s not limited to anyone based on childbirth history. While some women have minimal symptoms, for others adenomyosis causes ongoing pelvic pain and prolonged, heavy periods that make menstruation a recurring during menstruation affecting daily life.
3. Signs and symptoms: how it shows up during your cycle
Common symptoms include:
- Very painful periods (dysmenorrhea) that get worse over time.
- Heavy or prolonged bleeding (menorrhagia).
- A sense of pelvic pressure, bloating, or a bulky-feeling uterus.
- Pain during sex.
- Sometimes infertility or difficulty conceiving in some patients.
Because the abnormal tissue bleeds inside the muscle wall, adenomyosis is a frequent cause of heavy, painful periods — a clear example of a problem during menstruation. Not everyone with adenomyosis has symptoms; some cases are found incidentally on imaging or after hysterectomy.
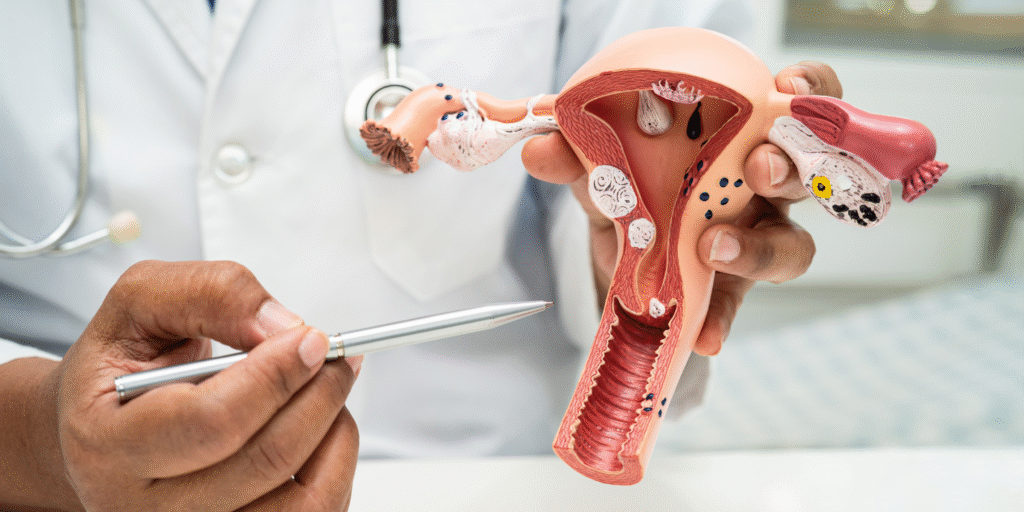
4. How doctors diagnose adenomyosis
No single blood test confirms adenomyosis. Diagnosis usually combines:
- A careful history and pelvic exam,
- Transvaginal ultrasound (often the first imaging test), and
- MRI in unclear or complex cases.
Ultrasound is the preferred initial imaging tool because it’s widely available and accurate, while MRI can be used when findings are unclear or if surgery is being planned. Definitive confirmation historically required examining the uterus after hysterectomy, but modern imaging often gives a reliable working diagnosis.
5. Treatment options — from pills to procedures
Treatment is tailored to your symptoms, age, fertility plans, and how much the condition affects your life. Options include:
First-line and medical treatments
- Nonsteroidal anti-inflammatories (NSAIDs) for menstrual cramp relief (ibuprofen, naproxen).
- Hormonal contraceptives (combined birth control pills or progestin-only methods) to reduce bleeding and pain.
- Levonorgestrel-releasing intrauterine device — very effective at decreasing heavy bleeding and pain for many women and is often recommended as a first-line long-term option when fertility preservation is desired.
- Tranexamic acid (during heavy days) to reduce blood loss for those who can use it safely.
These medical approaches frequently reduce the problem during menstruation and may be tried first.
Minimally invasive and targeted procedures
- Uterine artery embolization (UAE) — blocks blood supply to problematic areas and can reduce bleeding and pain for some patients.
- Focused ultrasound (MRgFUS) — a noninvasive option at specialized centers; heats and destroys adenomyotic tissue under MRI guidance.
- Adenomyomectomy (surgical removal of adenomyotic tissue) — available for selected patients who want uterine-sparing surgery; technically demanding.
Definitive treatment
- Hysterectomy (removal of the uterus) is the only permanent cure for adenomyosis and may be considered when symptoms are severe, medical therapies fail, and childbearing is complete. In some cases, hysterectomy is the best option for improving quality of life.
Choosing the right path: Your gynecologist will weigh severity, fertility desires, medical history and response to prior treatments. Shared decision-making is essential.
6. Adenomyosis and fertility — what the evidence says
Research suggests adenomyosis can be associated with reduced fertility, lower implantation rates and increased miscarriage risk in some cases — though the relationship is complex and depends on the extent and location of disease. If you’re trying to conceive, tell your specialist so fertility-preserving options can be prioritized. A recent literature review summarizes current understanding and treatment approaches for patients facing infertility with adenomyosis.
7. Living better: practical steps for a recurring problem during menstruation
While you work with your doctor to find the right medical plan, these practical steps often help:
- Track your cycle and symptoms. Note bleeding amount, pain intensity, and sick days. This helps your clinician choose treatments.
- Use heat and gentle movement. Heat packs and light exercise can reduce cramping.
- Optimize pain meds. Use NSAIDs timed for the start of cramping; they are more effective when started early.
- Check iron levels. Heavy periods can cause iron deficiency — ask for a hemoglobin and ferritin check and consider iron supplements if low.
- Consider the LNG-IUD. For many women it cuts bleeding and pain substantially and avoids major surgery.
- Talk about mental health. Chronic pain and heavy bleeding take an emotional toll — counselling or support groups can help.
If your periods stop you from doing daily activities, it’s time to see a gynecologist.
8. Helpful enhancements: quick tools you can use
Symptom checklist (bring this to your appointment):
- How long do periods last?
- How many pads/tampons per day on heavy days?
- Pain score (0–10) on worst days?
- Interference with work or sleep?
- Prior treatments tried and outcomes?
Questions to ask your doctor:
- Could my symptoms be caused by adenomyosis or something else (fibroids, endometriosis)?
- Do I need an ultrasound or MRI?
- Is the LNG-IUD a good option for me?
- What are the pros/cons of uterine-sparing surgery versus hysterectomy?
How will this affect my fertility or pregnancy plans?
9. When to see a specialist
Make an appointment with a gynecologist if:
- Period pain or bleeding prevents normal activities, or
- You soak through sanitary protection frequently, or
- You have anemia symptoms (weakness, breathlessness), or
- Pain during sex or persistent pelvic discomfort occurs.
If you live near or would like specialized care, Karthika Woman and Child Care offers evaluation and treatment for menstrual disorders and adenomyosis. Visit karthikawomanandchildcare.in to learn about appointments and services.
Author & review box
Written by: A senior gynecologist with 10 years’ clinical experience in menstrual and uterine disorders, Karthika Woman and Child Care.
Reviewed by: Multidisciplinary team, Karthika Woman and Child Care.
Clinic: Karthika Woman and Child Care — karthikawomanandchildcare.in
Contact: +91 99459 26987