By Divya Venugopalan | Karthika Woman and Childcare
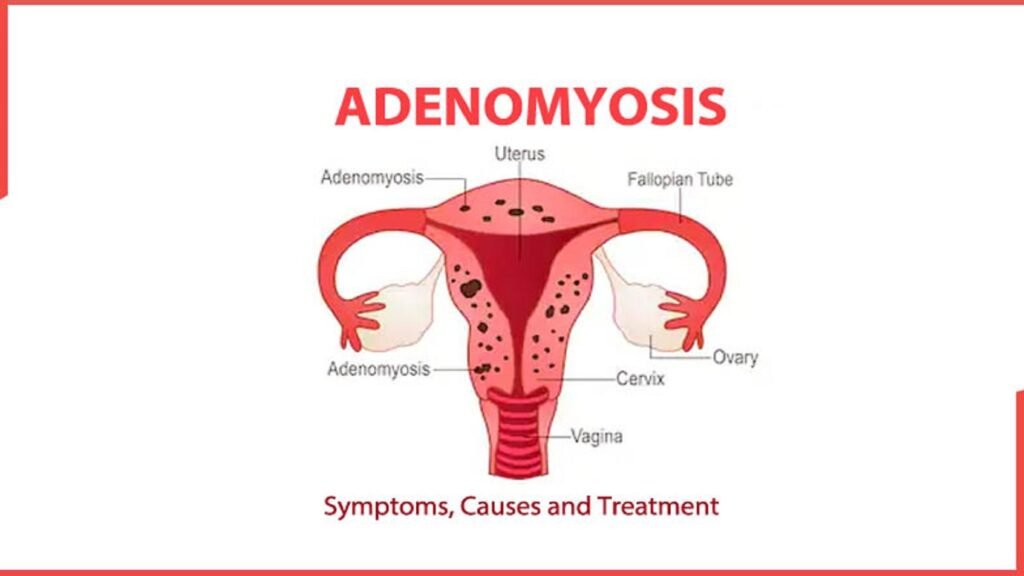
Adenomyosis is a gynecological condition in which endometrial‑like tissue infiltrates the uterine muscle (myometrium), resulting in symptoms such as heavy menstrual bleeding, painful periods, pelvic pain, and sometimes fertility difficulties. Adenomyosis commonly affects women in their 30s to 50s, but with better imaging via MRI and transvaginal ultrasound, it is now increasingly diagnosed in younger women as well.
Treatment options for adenomyosis fall into two major categories: medical (non‑surgical) and surgical/procedural. The right approach depends on the patient’s symptoms, age, desire for fertility, and severity of disease.
Medical (Non‑Surgical) Treatments for Adenomyosis
1. NSAIDs (Non‑Steroidal Anti‑Inflammatory Drugs)
For women with mild pain who are planning pregnancy or avoiding hormones, NSAIDs such as ibuprofen or naproxen are commonly used to reduce prostaglandin‑mediated dysmenorrhea and heavy bleeding. They offer symptomatic relief but do not modify the disease itself.
2. Tranexamic Acid
Tranexamic acid helps to control heavy menstrual bleeding by reducing fibrinolysis. When combined with NSAIDs or hormonal therapy, it can cut menorrhagia significantly, providing non‑hormonal relief for select patients
3. Levonorgestrel‑Releasing Intrauterine Device (LNG‑IUS)
The LNG‑IUS (e.g. Mirena) is widely regarded as the first‑line medical treatment for adenomyosis in women not seeking pregnancy. Delivering levonorgestrel directly to the uterus, it reduces heavy menstrual bleeding, pain, and often leads to uterine shrinkage. Symptom improvement is seen in up to 90% of users, with high satisfaction and quality‑of‑life gains comparable to hysterectomy . Guidelines from NICE UK and Asia emphasize its use as first-line therapy.
4. Combined Oral Contraceptives (COCs) and Progestins
Oral contraceptives and synthetic progestins (e.g. norethisterone acetate, dienogest) can reduce menstrual bleeding and dysmenorrhea. While COCs suppress ovulation and endometrial proliferation, evidence for effect on adenomyotic lesions or uterine size is inconclusive. Dienogest, in particular, has shown efficacy in reducing pain and improving quality of life, though uterine shrinkage is modest.
5. GnRH Agonists and Antagonists
GnRH Agonists (e.g. leuprolide acetate):
By inducing a hypoestrogenic state, GnRH agonists reduce uterine and lesion volume, relieve pain and bleeding, and may promote regression of adenomyosis lesions. However, due to side effects like bone density loss and menopausal symptoms, they are typically used short‑term or as pre‑fertility adjuncts.
GnRH Antagonists (e.g. elagolix, linzagolix):
These newer agents offer immediate suppression of gonadotropins without the initial hormone flare. They enable dose titration and may be better tolerated with less bone loss and menopausal side‑effects. Emerging data show promise in reducing symptoms and uterine size in adenomyosis, though longer‑term studies are ongoing.
6. Aromatase Inhibitors
By blocking local estrogen production (aromatase P450), letrozole and others can reduce adenomyotic volume and symptoms. In pilot studies combined with GnRH agonists, they achieved reductions in both uterine and adenomyoma sizes and alleviated pain .
7. Experimental & Emerging Therapies
- Oxytocin antagonists (e.g. epelsiban) are under investigation, targeting overexpressed oxytocin receptors in adenomyotic uteri. Early studies show tolerability, but clinical efficacy in real‑world adenomyosis is yet to be determined.
- Selective Progesterone Receptor Modulators, anti‑platelet therapy, valproic acid, and other novel agents are also being explored, although they remain experimental.
Surgical & Procedural Options for Adenomyosis
If symptoms are severe, fertility is not a priority, or medical therapy has failed, surgical or interventional solutions may be offered. These range from minimally invasive interventions to definitive hysterectomy.
1. Hysterectomy (Definitive Treatment)
Hysterectomy remains the only definitive cure for adenomyosis, offering the highest rates of symptom resolution. It’s most suitable for women who have completed childbearing or do not wish to preserve fertility. While highly effective for bleeding and pain, persistent symptoms can occur due to coexisting endometriosis, central pain sensitization, or retained ovaries.
2. Uterine‑Sparing Excisional Surgery (Adenomyomectomy)
- Focal adenomyosis (adenomyoma) can sometimes be removed via wedge resection or partial excision, preserving the uterus. In experienced hands, pain and bleeding reduction rates are significant, and pregnancy rates of ~60 % have been reported. However, risks include uterine rupture in future pregnancies (~4 %) and recurrence rates up to ~9–20 % .
- Diffuse adenomyosis can be treated using techniques such as the triple‑flap method or real‑time ultrasound guided excision, sometimes combined with LNG‑IUS placement. These are technically challenging and outcomes vary .
3. Uterine Artery Embolization (UAE)
UAE is a minimally invasive radiologic procedure that occludes uterine arterial supply, causing ischemic necrosis of adenomyotic lesions. It has shown symptom improvement in up to 83 % of women, especially when adenomyosis coexists with fibroids. Recovery is relatively quick, and it avoids open surgery. However, risks include premature ovarian failure, reduced fertility, and higher rates of repeat procedures. Guidelines from NICE, SOGC, and Asian Society support its use for symptomatic adenomyosis in women not desiring fertility.
4. Endometrial/Endomyometrial Ablation & Electrocoagulation
These non-excisional techniques destroy or thin the uterine lining to reduce bleeding and some pain. While effective for heavy menstrual bleeding, they carry a risk of worsening pain and are not suitable for women wishing to conceive. Success rates vary widely (~57 to 98 %) with recurrence rates up to ~30 % depending on technique completeness (.
5. High‑Intensity Focused Ultrasound (HIFU) and Other Ablative Technologies
- MRI-guided or ultrasound-guided HIFU uses focused ultrasound waves to thermally ablate adenomyotic tissue. It’s non-invasive, outpatient, and preserves the uterus. Small studies show symptom relief, but recurrence is not uncommon, and randomized controlled trials remain lacking. Availability is growing in Europe and Asia, though in some countries (e.g., the US) coverage is limited.
- Radiofrequency ablation (RFA) and microwave ablation are also being studied, with early data indicating reduced pain and bleeding, though long‑term fertility data are limited.
Choosing the Right Treatment: Factors to Consider
Treatment selection for adenomyosis is highly individualized, with key considerations including:
- Desire for future fertility: Women wishing to conceive favor conservative options (NSAIDs, LNG-IUS, excisional surgery, or even short-term GnRH therapies).
- Severity of symptoms: Heavy bleeding and debilitating pain may warrant escalating from medical therapy to interventional procedures.
- Disease extent: Focal adenomyosis may be suited to excision, while diffuse disease may respond better to systemic or ablative approaches.
- Age and comorbidity: Older women, or those with contraindications to hormonal therapy, may be guided toward uterine-sparing ablation or hysterectomy.
- Tolerance of side effects: GnRH agents may cause menopausal symptoms; LNG-IUS can cause spotting; UAE may impact ovarian reserve .
Summary Comparison Table
| Treatment Type | Representative Options | Benefits | Limitations |
| Medical (Hormonal/Analgesic) | NSAIDs, Tranexamic acid, LNG‑IUS, COCs, Dienogest, GnRH agonists/antagonists, Aromatase inhibitors | Symptom control, fertility preservation, minimally invasive | Recurrence after stopping treatment, side effects, limited lesion regression |
| Uterine‑Sparing Surgery | Adenomyomectomy (wedge, triple‑flap), excision | Relief of bleeding/pain, fertility preservation possible | Technically challenging, risk of uterine rupture, recurrence |
| Interventional Radiology / Ablation | UAE, HIFU, RFA, endometrial ablation | Less invasive, quicker recovery, symptom relief | May impair fertility, variable long‑term efficacy, recurrence |
| Definitive Surgery | Hysterectomy (total or subtotal) | Permanent symptom resolution | Loss of fertility, surgical risks, possible persistent pain if endometriosis present |
Advice for Patients at Karthika Woman and Childcare
As you evaluate treatment options for adenomyosis, consider the following steps:
- Discuss your goals: Clarify whether preserving fertility is essential.
- Confirm diagnosis thoroughly: Transvaginal ultrasound is first‑line; MRI can further characterize the disease type and location.
- Start with medical therapy: For most patients without urgent surgical needs, the LNG‑IUS is often the most effective first-line therapy.
- Use systemic medications judiciously: NSAIDs, COCs, dienogest, GnRH agents, or aromatase inhibitors can be employed based on tolerance and priorities.
- Escalate to procedural options as needed: If bleeding or pain remains severe, consider UAE or minimally invasive ablative methods. For fertility-focused patients with focal disease, adenomyomectomy may be advised.
- Reserve hysterectomy for refractory cases: When conservative approaches fail and fertility is no longer desired, hysterectomy remains the only definitive cure.
- Consider combination approaches: For example, adenomyomectomy plus LNG‑IUS or pre‑surgical GnRH therapy may optimize outcomes in select cases .
Final Thoughts
Adenomyosis is a complex and often under‑recognized condition that significantly affects quality of life. While hysterectomy remains the only curative option, a range of medical therapies (especially LNG‑IUS and hormonal agents) and uterine-sparing procedures (such as excision, UAE, HIFU, or ablation) offer effective symptom control and fertility preservation for many women.
Consultation with a gynecologist specialized in adenomyosis, ideally in a multidisciplinary setting, helps identify the optimal, evidence‑based route tailored to each patient’s needs and preferences.
📞 How to Book
If you’re searching for a women specialist clinic near me for fertility care, here’s how to reach Dr. Venugopalan at Cloudnine:
- Phone:+91 99728 99728 (Cloudnine booking desk)
- Book via app/website:https://karthikawomanandchildcare.in/
- Clinic Locations:
- Thanisandra Main Road, Bengaluru
- HRBR Layout, Bengaluru