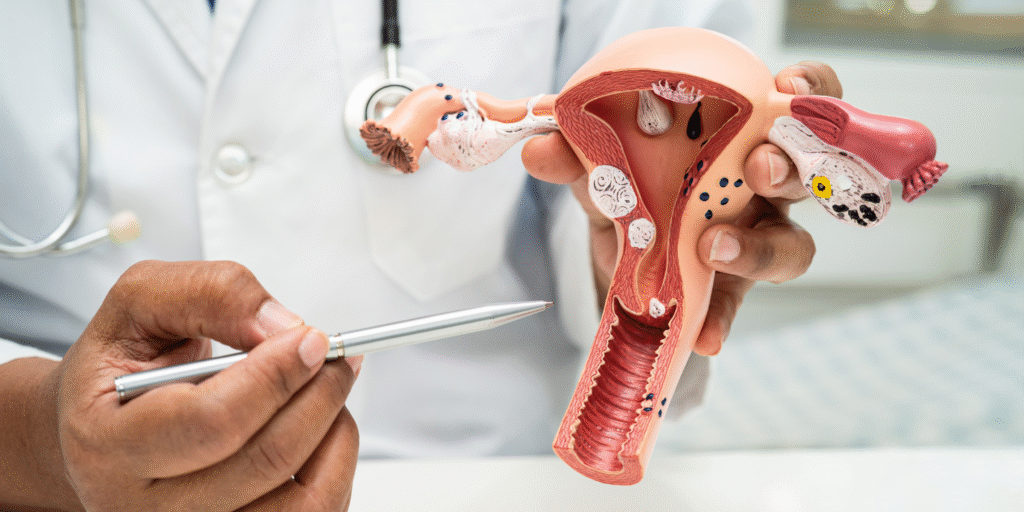
Adenomyosis is a hormonal‑sensitive condition of the uterus, in which endometrial tissue grows into the muscular wall (myometrium), triggering symptoms like heavy menstrual bleeding, chronic pelvic pain, painful periods, and reproductive issues. In this blog, we explore how hormonal imbalances, particularly estrogen and progesterone, influence the progression of adenomyosis, and what patients and clinicians—especially at Karthika Woman & Childcare—should know
1. Why hormones matter in adenomyosis
The uterine endometrium normally proliferates and sheds in response to cyclic levels of estrogen and progesterone. In adenomyosis, ectopic endometrial tissue within the myometrium responds abnormally, creating inflammation, vascular changes, and enhanced growth. Excess estrogen and inadequate progesterone action can fuel this pathological growth.
Symptoms like heavy periods (menorrhagia) and pelvic pain often coincide with hormonal highs—especially estrogen dominance. Women nearing menopause or those on estrogen‑only therapies may experience worsening progression of adenomyosis.
1. Why hormones matter in adenomyosis
The uterine endometrium normally proliferates and sheds in response to cyclic levels of estrogen and progesterone. In adenomyosis, ectopic endometrial tissue within the myometrium responds abnormally, creating inflammation, vascular changes, and enhanced growth. Excess estrogen and inadequate progesterone action can fuel this pathological growth.
Symptoms like heavy periods (menorrhagia) and pelvic pain often coincide with hormonal highs—especially estrogen dominance. Women nearing menopause or those on estrogen‑only therapies may experience worsening progression of adenomyosis.
2. Estrogen: fuel for disease expansion
a) Enhanced tissue growth
Estrogen acts as a mitogen for endometrial tissues. In adenomyosis, estrogen promotes glandular hyperplasia and myometrial smooth muscle proliferation, increasing uterine volume and symptom severity.
b) Pro‑inflammatory effect
High estrogen promotes inflammation via elevated cytokines (e.g. IL‑6, TNF‑α) and angiogenic factors (VEGF), which contribute to pelvic pain and lesion expansion.
c) Local estrogen production
Ectopic lesions can convert androgens into estrogen via aromatase, resulting in intralesional estrogen synthesis—creating a localized hyper‑estrogenic microenvironment that sustains adenomyosis.
3. Progesterone: protective but often impaired
a) Progesterone resistance
Although progesterone normally counterbalances estrogen, adenomyotic tissues often exhibit progesterone receptor downregulation, reducing responsiveness. This results in ineffective endometrial shedding, accumulating lesions over time.
b) Imbalanced ratio
A disrupted estrogen
ratio (with excess estrogen and insufficient progesterone action) promotes proliferation, poor differentiation, and tissue remodeling, accelerating disease progression.
4. Hormonal life‑stages and adenomyosis
a) Reproductive years
Most patients develop adenomyosis between ages 30–50. During this phase, cyclic estrogen peaks and luteal phase progesterone dips may deepen symptoms.
b) Perimenopause and menopause
As ovulatory cycles become irregular, estrogen can remain elevated relative to progesterone—perimenopausal estrogen dominance aggravates adenomyosis. After menopause, estrogen levels decline and lesions often regress naturally.
5. Hormonal influences on symptoms and fertility
a) Heavy menstrual bleeding
Estrogen‑driven endometrial overgrowth leads to thickened lining. Progesterone resistance impairs proper shedding. The result is menorrhagia, often requiring iron supplementation or surgical intervention in advanced adenomyosis.
b) Pelvic pain
Estrogen stimulates nerve growth (nerve fiber density higher in lesions), while inflammatory mediators and prostaglandins cause dysmenorrhea and chronic pelvic pain.
c) Infertility and fertility challenges
Adenomyosis distorts uterine contractility and endometrial receptivity. Hormonal imbalance exacerbates poor implantation, recurrent miscarriage, and subfertility.
6. Diagnosis and hormonal assessment
a) Imaging
Transvaginal ultrasound and MRI help assess uterine size, junctional zone thickness, and adenomyotic nodules—often correlated with estrogen‑driven uterine enlargement.
b) Hormonal evaluation
Assessment of serum estrogen levels, progesterone, and sometimes estradiol
ratio, can guide therapeutic decisions.
c) Biopsy/predictive markers
Recent studies highlight receptor expression (estrogen receptors ERα/β, progesterone receptors PRA/PGR-B) and molecular markers (Ki‑67 proliferation index) as diagnostic and prognostic factors in adenomyosis progression.
7. Hormonal treatments targeting progression
a) Combined oral contraceptives (COCs)
COCs suppress ovulation, lower estrogen peaks, and create regular withdrawal bleeding. They help reduce pain, bleeding, and may slow lesion progression.
b) Progestin therapies
Options include levonorgestrel intrauterine system (LNG‑IUS), oral progestins, or injectables like Depot‑Medroxyprogesterone. They induce decidualization of ectopic endometrium and help control bleeding and pain, despite some degree of progesterone resistance.
c) Gonadotropin-releasing hormone (GnRH) analogs
These suppress ovarian estrogen production, inducing hypoestrogenism. Effective for symptom control and lesion shrinkage over short term. “Add‑back” estrogen/progestin may be needed to manage side effects.
d) Aromatase inhibitors
Rarely used alone, but can reduce local estrogen production in adenomyotic tissues for post‑menopausal or refractory cases.
e) Selective progesterone receptor modulators (SPRMs)
Emerging therapies such as ulipristal acetate aim to modulate receptor action—still under investigation for adenomyosis.
8. Lifestyle, diet & natural hormonal support
Although not sufficient to halt progression alone, lifestyle choices can modulate hormonal balance:
- Balanced diet: high in fiber, phytoestrogens (flaxseed, soy), and low‑fat dairy to support estrogen metabolism.
- Regular exercise: reduces peripheral estrogen production and inflammation.
- Weight management: adipose tissue produces estrogen; weight control helps lower overall estrogen load.
- Stress reduction: cortisol can impact gonadotropin release and cyclic hormones—stress management may improve hormonal balance.
Herbal supplements (e.g., chasteberry, dong quai) may offer mild modulation—but should only be used under supervision due to hormonal potency.
9. Monitoring hormonal response and progression
At Karthika Woman & Childcare, Dr. Karthika and her team use a personalized approach:
- Baseline hormone panel: estradiol, progesterone, thyroid, and prolactin to rule out confounders.
- Imaging follow‑up: ultrasound or MRI after 6–12 months to evaluate junctional zone thickness and uterine volume.
- Symptom tracking: menstrual diary, pain scores, bleeding logs.
- Treatment adjustments: based on hormonal response, imaging, and patient preferences.
10. When hormones alone aren’t enough
For women desiring fertility or those whose symptoms persist despite hormonal therapies, surgical or interventional options may be considered:
- Uterine artery embolization (UAE): reduces vascular supply to adenomyotic lesions, shrinking them. Hormone reduction may enhance effect.
- Conservative surgery: adenomyomectomy (removal of adenomyotic tissue) combined with hormonal therapy can preserve fertility.
- Hysterectomy: for patients who have completed family and want permanent relief, especially if hormone therapy is contraindicated.
- Uterine artery embolization (UAE): reduces vascular supply to adenomyotic lesions, shrinking them. Hormone reduction may enhance effect.
Contact Us – Karthika Woman & Childcare
Address:CloudnineThanisandra Bengaluru
Sahakaranagar Bengaluru
Contact Numbers:+91 99728 99728
Email:info@karthikawomanandchildcare.in
Website:https://karthikawomanandchildcare.in/
Contact Us – Karthika Woman & Childcare
Understanding the hormonal influence on adenomyosis progression is critical for effective management. Estrogen excess and progesterone resistance drive disease growth, symptoms, and fertility challenges. Hormonal therapies—COCs, progestins, GnRH analogs—remain first‑line treatment, often combined with lifestyle strategies. When managed in a specialized centre like Karthika Woman & Childcare, patients benefit from a holistic approach—diagnosis, treatment, follow‑up, and surgical options when needed.
To learn more or schedule a consultation, don’t hesitate to reach out to Karthika Woman & Childcare at the contact information above.