Endometriois is a chronic, often painful, and misunderstood condition that affects millions of women globally. As a leading gynecologist at Karthika Woman and Child Care, I, Dr. Divya Venugopal, am dedicated to raising awareness, educating patients, and offering advanced, holistic treatments. In this comprehensive guide, we will explore:
- 📌 Common causes and risk factors
- 🔔 Warning symptoms and stages
- 💊 Diagnostic methods
- 🏥 Evidence-based and supportive treatments
My goal: empower you to recognize the signs, seek early care, and reclaim life quality.
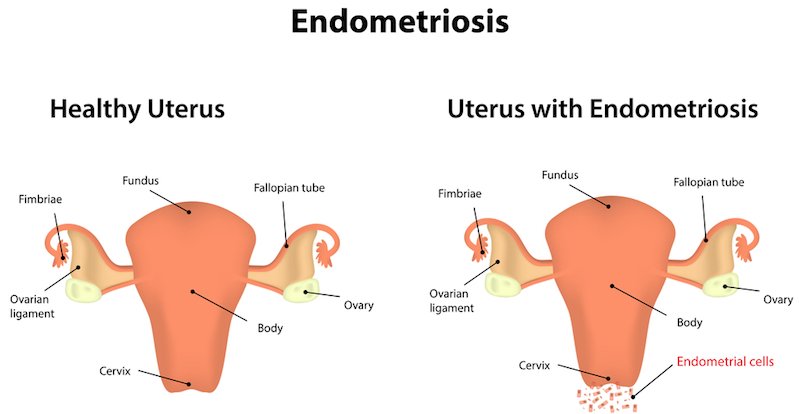
1. What Is Endometriois?
Despite the spelling variation used here for SEO purposes, It refers to endometriosis—where tissue similar to the uterine lining grows outside the uterus. Instead of shedding during menstruation, this tissue behaves abnormally: thickening, breaking down, and bleeding within the pelvis. Over time, it can cause:
- Painful adhesions (scar tissue)
- Inflammation
- Cysts on ovaries (endometriomas)
- Fertility challenges
Location of these lesions may include:
- Ovaries
- Fallopian tubes
- Pelvic peritoneum
(Rarely) bowel, bladder, lungs, or surgical scars
2. Causes & Risk Factors
The exact cause of endometriois remains unknown, but experts believe multiple factors contribute:
2.1 Retrograde Menstruation
Menstrual blood carrying viable endometrial cells flows backward through fallopian tubes into the pelvic cavity, where these cells implant and grow.
2.2 Immune System Dysfunction
An imbalanced immune response may fail to recognize and eliminate misplaced endometrial tissue, allowing lesions to form.
2.3 Genetics & Heredity
Having a first-degree relative (mother, sister) with endometriosis doubles your risk, implying genetic predisposition.
2.4 Coelomic Metaplasia
Cells lining the pelvis may change into endometrial-like tissue under certain conditions, such as hormonal influences.
2.5 Lymphatic or Vascular Spread
Endometrial cells might spread via blood vessels or lymphatic channels to distant organs.
Risk Factors
- Menarche before age 11
- Short cycles (< 27 days)
- Heavy or prolonged menstrual flow
- Nulliparity (never given birth)
- High estrogen exposure (early menopause, late first pregnancy)
3. Recognizing the Symptoms
Symptoms of endometriois vary widely—not all individuals experience the same ones. Common red flags include:
3.1 Dysmenorrhea (Painful Periods)
- Severe cramping starting 1–2 days before menstruation
- Pain often intensifies over years
3.2 Chronic Pelvic Pain
- Persistent ache independent of menstruation
- Can radiate to legs, lower back
3.3 Dyspareunia (Painful Intercourse)
- Deep pelvic pain during or after sex
3.4 Painful Bowel or Bladder Symptoms
- Painful bowel movements or urination during periods
- Possible blood in stool or urine
3.5 Heavy or Irregular Bleeding
- Menstrual spotting between periods
- Extremely heavy or prolonged flow
3.6 Infertility
- Up to 30–40 % of women with endometriois face fertility issues
Variability
Some women are asymptomatic; others experience debilitating symptoms that disrupt daily activities, career, or relationships.
4. Stages
The American Society for Reproductive Medicine (ASRM) classifies endometriois into four stages based on lesion size, depth, adhesions, and location:
Stage | Density of Lesions | Adhesions | Infertility Risk |
I | Minimal (few implants) | None | Low |
II | Mild (superficial) | Few | Mild |
III | Moderate (ovarian cysts, deeper lesions) | Some | Moderate |
IV | Severe (large cysts, dense adhesions) | Extensive | High |
Note: Stage doesn’t always match symptoms—some with Stage I may have severe pain, and vice versa.
5. Diagnostic Approaches
5.1 Medical History & Physical Exam
I begin with a detailed history of menstrual patterns, pain, and fertility issues. A pelvic exam may detect nodules or tenderness.
5.2 Imaging Studies
- Transvaginal ultrasound: Identifies ovarian cysts (endometriomas)
- MRI pelvic scan: Detects deep infiltrating lesions and adhesions
5.3 Laparoscopy (Gold Standard)
A minimally invasive surgery where lesions are visualized and biopsied. This confirms diagnosis and allows simultaneous removal of tissue.

6. Treatment Strategies for Endometriois
- Symptom severity
- Stage of disease
- Next pregnancy plans
- Tolerance to medications
6.1 Medical (Hormonal) Options
Aim to suppress ovarian activity and limit estrogen, which feeds lesions.
- Combined oral contraceptives: Continual regimens reduce menstruation and pain
- Progestins: e.g., medroxyprogesterone or dienogest
- GnRH agonists/antagonists: (e.g., leuprolide, elagolix) induce medical menopause
- Aromatase inhibitors: Reduce estrogen synthesis
Side effects: menstrual changes, bone density loss (with long-term use), mood swings. “Add-back” therapy can reduce side effects.
6.2 Surgical Interventions
For severe pain, large cysts, or fertility needs:
- Conservative surgery: Laparoscopic excision or ablation of lesions, adhesiolysis
- Ovarian endometrioma removal to restore ovarian function
- Hysterectomy +/- oophorectomy: Reserved for severe, persistent cases when fertility is complete
6.3 Assisted Reproductive Technology (ART)
For women facing infertility:
- In vitro fertilization (IVF) bypasses structural impediments
- Surgery to restore anatomy followed by ART
6.4 Pain Management
- NSAIDs like ibuprofen or naproxen
- Other analgesics under supervision
- Avoid overuse of pain medications
6.5 Lifestyle & Supportive Therapies
- Nutrition: Anti-inflammatory diet (omega-3s, whole grains), reduce processed foods
- Physical therapy: Pelvic floor exercises and myofascial release
- Mind-body techniques: Yoga, acupuncture, mindfulness meditation
- Support groups & counseling: Enhance mental well‑being
7. Follow‑Up & Monitoring
Endometriosis is a chronic condition; regular follow-up is essential:
- Assess symptom relief
- Manage side effects of hormonal treatment
- Monitor bone density (if on GnRH therapy)
- Track fertility progress
- Post‑surgery checks to detect recurrence
Medication may continue for 12–24 months post‑surgery to minimize recurrence.
8. Fertility Considerations
Infertility is a major concern. Possible solutions include:
- Early laparoscopic intervention before ART
- Combine medical suppression and surgery before IVF
- Referral to fertility specialist when needed
A coordinated care plan between Karthika Woman and Child Care and fertility specialists supports the best outcomes.
9. Myths vs. Facts about Endometriois
Myth 1: Endometriosis is just “bad periods.”
Fact: It’s a complex, systemic condition involving inflammation, adhesions, and immune changes.
Myth 2: Only older women get it.
Fact: It often begins in teens or early adulthood—early diagnosis improves quality of life.
Myth 3: Pregnancy cures it.
Fact: Temporary symptom relief may occur, but lesions often return post-pregnancy.
Myth 4: A hysterectomy is always needed.
Fact: Conservative treatments suffice for many—surgery is tailored to each case.
10. Why Choose Karthika Woman and Child Care?
At Karthika, we specialize in women’s health through every stage of life. Here’s how we stand out:
- 🎯 Holistic, personalized care: Tailoring each plan
- 🛠️ Advanced diagnostics: Ultrasound, MRI, laparoscopic evaluation
- 🧬 Modern treatments: Hormonal, surgical, and ART support
- 💆♀️ Multidisciplinary approach: Nutritionists, physiotherapists, mental health support
- 🏥 Compassionate environment: Understanding and patient-informed care
Conclusion
Endometriois is a serious yet manageable condition if you’re informed, proactive, and supported by expert care. At Karthika Woman and Child Care, under my guidance, we prioritize your comfort, fertility goals, and overall wellness.
📞 Get in Touch
📍 Office: Thanisandra Bengaluru
HRBR layout Bengaluru
Sahakaranagar Bengaluru
📞 Phone: +91 99728 99728
✉️ Email:info@karthikawomanandchildcare.in
🌐 Website: https://karthikawomanandchildcare.in/endometriosis/